Stay Informed
Follow us on social media accounts to stay up to date with REHVA actualities
|
| , |
|
|
Jacob Bueno de Mesquita | Núria Casquero-Modrego | Iain Walker | Brennan Less | Brett Singer |
Assistant Professor | Roger Williams Universityjbuenodemesquita@rwu.edu | Postdoctoral ResearcherNuriaCM@lbl.gov | Staff ScientistISWalker@lbl.gov | Technological ResearcherBDLess@lbl.gov | Senior ScientistBCSinger@lbl.gov |
While this article presents a condensed overview, complete references and more details can be found in: Mesquita, P., Casquero-Modrego, N., Walker, I., Less, B., & Singer, B. (2023). Quantifying the Potential Health Impacts of Unvented Combustion in Homes–A Meta-Analysis.
The primary consumers of fossil fuels in homes are: heating, hot water, cooking and clothes drying. Heating, hot water and clothes drying are required to have a vent to outside and only contaminate indoor air if their venting system fails. This venting combustion products contributes to outside air pollution that can then enter a home by natural infiltration or ventilation. However; this article focuses on cooking and unvented heaters that are direct indoor sources of combustion-related contaminants.
The inhalation of fossil fuel combustion products leads to a range of adverse population health effects. Particles are the most important contaminant of concern for health impacts, at least from Disability Adjusted Life Year (DALY) perspective, however, most particle exposure is from non-residential sources such as transport, agriculture and industry. This article focuses on NO₂ because NO₂ is an irritant to the respiratory tract, and even short-term exposures can irritate the airways, drive inflammation, and lead to acute and chronic disease, especially among those with asthma. Previous meta-analyses have shown that the effect of NO₂ was independent from PM, suggesting that NO₂ can drive health effects on its own.
Meta-analyses of epidemiological studies have shown clear relationships with asthma development and have enabled modelling studies estimating the broader population impacts of reducing NO₂ exposures. A synthesis of the available literature on gas stove use (Lin et al., 2013) found correlations with the two health outcomes they studied, asthma development and wheeze in children. This article provides a 10-year update to Lin et al, to build on existing dose-response findings through the inclusion of studies published through April 2023 that reported on a broader set of potential adverse health effects like hospitalization, asthma symptoms and medication use.
This study reviews research since the year 2000 on the health impacts associated with exposure to combustion-related contaminants in homes. We examined the literature related to interventions where gas combustion appliances were replaced, or effective engineering controls were implemented, including those where measured NO₂ was taken as the main exposure variable. The health outcomes primarily were associated with acute exposures and were categorized into 12 distinct categories: 1) asthma symptoms including wheeze, cough, shortness of breath, chest tightness, respiratory symptoms, nasal symptoms, and difficulty breathing; 2) asthma symptom scores including ordinal scores 0-3 (3 as the most severe and 0 as no symptom) for wheeze, cough, overall asthma symptoms, upper respiratory, and lower respiratory symptoms; 3) systemic symptoms including poor/fair health, diarrhea, vomiting, ear infection stomach ache, eczema, sensitization, allergies, nighttime waking, and steroid use; 4) healthcare visits that were not hospitalizations or emergency room visits or changes to asthma management; 5) hospitalization or emergency room visits, 6) medication use including asthma preventer and reliever use; 7) nonpharmaceutical interventions including limiting activity; 8) neurological disease development including schizophrenia; 9) absences from school; 10) all-cause mortality; 11) cardiovascular mortality; 12) respiratory mortality. We converted effect estimates with continuous, independent variables to effects per 20 ppb increase in NO₂.
The search yielded 29 studies including 10 meta-analyses, 12 observational studies and 7 randomized controlled trials (RCTs) or quasi-experimental studies. In total, these included 184 effect estimates for a variety of health outcomes.
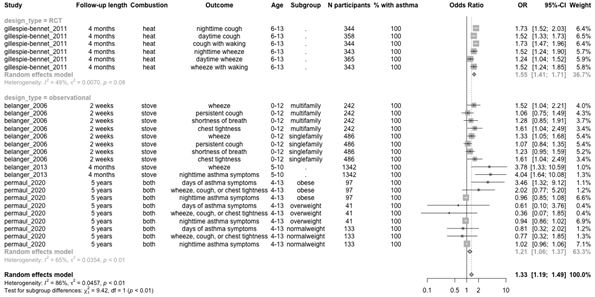
Asthma Symptoms and Symptom Scores. The presence of gas versus electric appliances, mediated by whether the gas appliances were vented (e.g., flue for gas heater), was associated with 1.16 times the odds of reporting asthma symptoms (95% CI 1.06-1.28). Table 1 summarizes odds ratios for a 20 ppb increase in average NO₂ exposure linked with combustion cooking and/or unvented heating. Each 20 ppb increase in NO₂ exposure linked with gas combustion was associated with 1.55 (95% CI 1.41-1.71) and 1.21 (95% CI 1.06-1.37) times higher odds of asthma symptoms, for RCTs and observational studies, respectively. The pooled OR of 1.33 (95% CI 1.19-1.49) may not be reliable given the lack of overlap in confidence intervals for RCTs and observational studies, yet the confidence interval ranges demonstrate a consistent, positive association with asthma symptom risk.
Systemic symptoms. We found evidence of a trend toward increased odds of systemic symptoms with gas combustion exposure, with a pooled OR of 1.25 (95% CI 1.04-1.51). The RCT effect estimates drove this trend in the pooled regression. Studies that reported effects as a function of continuous NO₂ exposure found similar results with OR of asthma medication use of 1.61 (95% CI 1.01-2.56) for each 20 ppb NO₂ increase.
Hospitalization, healthcare utilization and medication use. A number of other observational studies and RCTs reported on risks associated with residential gas combustion. A cross-sectional study with a 2-month prospective of survey data in Maryland showed a consistent, elevated trend toward higher risk of emergency room visit or hospitalization among children with bronchopulmonary dysplasia. Among those with respiratory support, the odds of hospitalization were 5.95 (95% CI 1.08-32.76) times greater for homes with gas combustion. Pooled analysis of studies evaluating the use of asthma medication showed 1.39 (95% CI 1.07-1.81) times higher odds with gas combustion exposure compared with electric appliance use or the addition of exhaust ventilation.
Table 1. Odds ratios for a 20 ppb increase in average NO₂ exposure linked with combustion cooking and/or heating.
A number of studies examined relationships between residential-level indoor NO₂ and population health risks and mostly used a continuous NO₂ exposure variable to evaluate risk of mortality, asthma incidence, emergency room visits, and hospitalizations. The risk of mortality was consistently elevated, with 95% CIs ranging up to 39% above the null (Table 2).
Table 2. Pooled meta-analysis all-cause mortality risk ratios for 20 ppb increases in indoor NO₂.
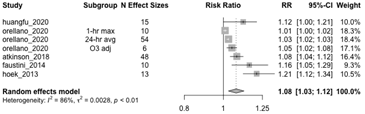
The study found that observational studies, RCTs, and meta-analyses showed consistent increased risks for asthma symptoms, asthma development, school absence, hospitalization, and emergency room visits. Overall, the health outcome with the most effect estimates for pooled analysis was the risk of asthma symptoms. The pooled estimates show a 6-28% (95% CI) increase in risk of symptoms for unvented gas heating or presence of gas stoves compared with flued heating or electric heat or stoves. For each 20 ppb increase NO₂ concentration, the odds of asthma symptoms increased 19-49% We observed elevated odds of asthma medication use across RCTs and observational studies with a pooled confidence interval of 7-81% higher odds with the presence of gas appliances. These results are consistent with both of these previous meta-analyses.
Dose-response relationships between human health, NO₂ exposure, and other by-products of combustion are not well characterized in the literature. Furthermore, these relationships are mediated by numerous factors both inside and outside the built environment, including the presence and use of exhaust ventilation, the duration and types of food preparation, psychosocial stressors, and pre-existing health conditions. However, there is clear evidence of a wide range of health effects, even at low levels of exposure.
The effect estimates, and confidence intervals presented here provide a window of reasonable risk levels for a variety of health outcomes and mortality. Despite the various designs, geographic sites, length of follow-up, and study dates, we noted a level of consistency between the studies within the current meta-analysis, and with previous ones, which strengthens the level of confidence in our findings. Given the small sample sizes, the pooled effect estimates are sensitive to the addition of new studies, given the small sample size. However, the reported confidence intervals are likely to be robust and provide perhaps a more helpful quantitative measure of risk given the inherent uncertainties and limitations of the epidemiologic studies required to detect population health effects in real-world conditions.
While gas stoves and unvented gas heaters can readily produce increases in NO₂ concentration associated with adverse health effects, exhaust ventilation can reduce but not eliminate gas stove emissions (Sun & Singer, 2023).
This work was supported by the Assistant Secretary for Energy Efficiency and Renewable Energy, Building Technologies Office, of the U.S. Department of Energy under Contract No. DE-AC0205CH11231.
Lin, W., Brunekreef, B., & Gehring, U. (2013). Meta-analysis of the effects of indoor nitrogen dioxide and gas cooking on asthma and wheeze in children. International Journal of Epidemiology, 42(6), 1724–1737. https://doi.org/10.1093/ije/dyt150.
Sun, L., & Singer, B. C. (2023). Cooking methods and kitchen ventilation availability, usage, perceived performance and potential in Canadian homes. Journal of Exposure Science & Environmental Epidemiology. https://doi.org/10.1038/s41370-023-00543-z.
Follow us on social media accounts to stay up to date with REHVA actualities
0